Obsessive-Compulsive Disorder
Obsessive-Compulsive Disorder (OCD) is often misused to describe general preferences for order and cleanliness. However, OCD goes far beyond keeping your home tidy; it is an all-encompassing mental health condition that can severely impact an individual’s life and well-being. OCD can trap individuals in a relentless cycle of intrusive and unwanted thoughts and repetitive behaviours, making work, relationships, and other normal life difficult. By fostering a deeper understanding of the disorder and acknowledging the depth and severity of its symptoms, the healthcare sector and society can better support individuals living with OCD.
What is OCD?
Obsessive-Compulsive Disorder, abbreviated as OCD, is a chronic mental health disorder marked by intrusive and persistent unwanted “obsessions”. These obsessions are not everyday worries rooted in real-life concerns but are often intense, irrational fears or urges that dominate an individual’s mind, creating substantial distress. Individuals feel compelled to engage in repetitive behaviours or thought processes called “compulsions” to alleviate this anxiety. Despite temporary relief, these compulsions often reinforce the obsessions, entrapping individuals in a relentless cycle.
Is it obvious when someone has OCD?
Determining whether someone has OCD is not always straightforward. While some symptoms are outwardly visible, others remain internal and are not easily noticeable to others. Notably, the cognitive characteristics of OCD can be highly individualistic and encompass a range of behaviours and thought patterns. Individuals with OCD may also actively conceal their symptoms, fearing judgement or misunderstanding, which further complicates the identification process. Here are some of the common signs and symptoms of OCD which could point to the need for professional intervention:
Signs of OCD obsessions
- OCD intrusive thoughts: One of the central cognitive characteristics of OCD is the presence of persistent, unwanted, and often distressing thoughts, which are hard to dispel.
- Fear of contamination: This manifests as a severe phobia of germs, leading to an avoidance of perceived ‘contaminated’ places or objects.
Signs of OCD compulsions
- Repetitive behaviours: Engagement in compulsive behaviours such as hand washing, checking or counting, governed by rigid rules.
- Arranging and rearranging: The compulsive habit of constantly arranging and rearranging objects in meticulous order, disrupting daily functioning.
- Excessive cleaning: Spending excessive time in cleaning or washing routines, attempting to ease fears of contamination.
- Hoarding: Engaging in hoarding behaviours, including the unnecessary collection and storage of items, coupled with a reluctance to discard them.
- Seeking reassurance: A common symptom is constantly seeking reassurance from others, often concerning irrational fears and apprehensions.
While these signs are common in adults, it is important to note that childhood OCD might exhibit differently, with children possibly unable to articulate their fears or compulsions clearly. Recognising the symptoms early on in childhood OCD can facilitate timely intervention and support.
- Extreme doubt: Individuals with OCD often have an incessant and irrational doubt about their ability to complete tasks.
- Need for symmetry: An overpowering need for symmetry and order, desiring things to be arranged precisely.
- Aggressive thoughts: Harbouring violent thoughts against oneself or others, usually with no intention of executing them.
Signs of OCD compulsions
- Repetitive behaviours: Engagement in compulsive behaviours such as hand washing, checking or counting, governed by rigid rules.
- Arranging and rearranging: The compulsive habit of constantly arranging and rearranging objects in meticulous order, disrupting daily functioning.
- Excessive cleaning: Spending excessive time in cleaning or washing routines, attempting to ease fears of contamination.
- Hoarding: Engaging in hoarding behaviours, including the unnecessary collection and storage of items, coupled with a reluctance to discard them.
- Seeking reassurance: A common symptom is constantly seeking reassurance from others, often concerning irrational fears and apprehensions.
While these signs are common in adults, it is important to note that childhood OCD might exhibit differently, with children possibly unable to articulate their fears or compulsions clearly. Recognising the symptoms early on in childhood OCD can facilitate timely intervention and support.
Types of OCD
OCD is not a one-size-fits-all condition and can present in infinite forms and manifestations which can overlap. While there are many different types of OCD, the most common include:
Contamination
The most common form of OCD, Contamination OCD, centres on the fear of germ or chemical contamination. This leads to avoidance of places like public toilets, door handles, and hospitals and can result in compulsive behaviours such as excessive cleaning.
Mental contamination
Mental contamination occurs when individuals feel mentally ‘dirty’ due to moral impurity, unethical situations, or critical experiences. Unlike Contamination OCD, it typically involves people, not objects.
Checking
This OCD form involves repeated checking due to fears like harm, mistakes, or fire. It leads to constant checking of locks, appliances, and switches to prevent imagined disasters. The need for reassurance includes seeking validation from others and verifying details, significantly disrupting daily life.
Symmetry and ordering
In this OCD subtype, individuals obsessively seek perfect symmetry and order in objects, driven by discomfort and anxiety. Even minor imperfections cause distress, leading to an ongoing cycle of rearranging until things feel ‘right,’ significantly impacting daily life.
Ruminations/OCD intrusive thoughts
This type features recurrent, distressing, intrusive thoughts, often focused on moral or ethical dilemmas. Individuals obsessively ponder deep questions or ‘what ifs,’ leading to mental exhaustion and rituals or avoidance behaviours.
Relationship OCD
Relationship OCD involves persistent doubts and worries about romantic relationships. Individuals seek constant reassurance about trust and may cycle through breakups and reunions. Common fears include falling out of love, having the ‘right’ feelings, and unfounded anxiety about infidelity.
False Memory OCD
False memory OCD features intrusive thoughts that seem like real memories of events that never happened. These distressing ‘false memories’ can lead to self-doubt, moral conflicts, and extreme anxiety.
Hoarding
Hoarding OCD involves compulsive acquisition and an aversion to discarding items, even with little value. Fear of future needs leads to clutter and distress, severely impacting the person’s quality of life.
The Stages of OCD
An integral aspect of understanding OCD is recognising the cyclical nature of its occurrence. This cycle can be broken down into four main stages, frequently repeating, often making the person feel trapped in a relentless loop. Recognising the different stages of OCD is vital for gaining control over the symptoms and breaking the cycle of OCD.
1. Obsession
The cycle begins with the obsession phase, where intrusive and unwanted thoughts, images or urges invade the individual’s mind and cause distress, fear and anxiety. Notably, even if individuals can recognise these obsessions as irrational, they still feel powerless to control them.
2. Anxiety
Following the emergence of obsessive thoughts, the individual then becomes increasingly anxious, grappling with the distress induced by the obsessions. This stage is characterised by heightened fear and a desperate need to alleviate the distress, leading them to the next phase.
3. Compulsion
To cope with the mounting anxiety, individuals with OCD engage in specific behaviours or mental acts driven by a compelling need to reduce the anxiety stemming from their obsessive thoughts. The acts can include repetitive behaviours like hand-washing, checking or mental rituals such as praying, counting or repeating phrases in their mind.
4. Temporary relief
Finally, performing the compulsions brings temporary relief from the anxiety. However, this relief is short-lived, as the individual often realises the irrationality of their compulsions, leading to a return of anxiety, a resurgence of obsessive thoughts and the continuation of the cycle.
It is important to note that the cycle can vary significantly among individuals, with some experiencing more intense anxiety or engaging in more complex compulsions. It’s a dynamic process, with each stage influencing the other, thereby maintaining the vicious cycle of OCD.
What causes OCD?
Understanding the triggers and causes of OCD is essential in crafting a strategic approach to managing the disorder. These triggers can span a range of biological, environmental and personal factors, each contributing to the onset and exacerbation of OCD symptoms.
Biological factors
- Genetic predisposition: A family history of OCD or other anxiety disorders can increase an individual’s likelihood of developing OCD, suggesting a genetic component in the disorder’s onset.
- Brain chemistry and structure: Certain abnormalities in brain structure and an imbalance in neurotransmitters, mainly serotonin, have been suggested to play a role in the onset of OCD.
Environmental factors
- Stressful life events: Major life transitions, traumatic events, or high-stress periods can also catalyse OCD symptoms.
- Childhood trauma: Evidence suggests that traumatic childhood experiences, including abuse and neglect, can be linked to developing OCD later in life.
Personal factors
- Personality traits: Individuals with perfectionism or a high need for control might be more prone to developing OCD.
- Age: The onset of OCD frequently occurs in adolescence or early adulthood, but it can also develop during childhood.
Health-related triggers
- Infections: In rare instances, paediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) can trigger OCD in children.
Pregnancy and postpartum: Hormonal fluctuations during pregnancy or postpartum can sometimes trigger a type of OCD known as perinatal OCD.
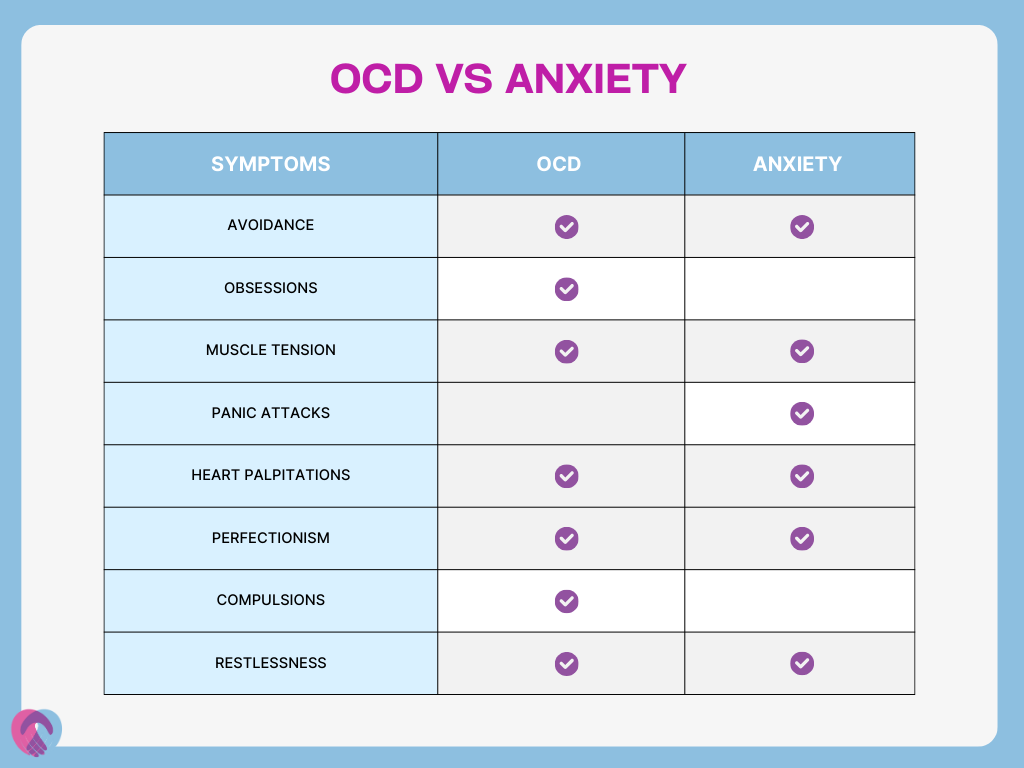
OCD and anxiety
OCD and anxiety disorders commonly co-occur which can complicate symptoms and management and take a major strain on an individual’s health and quality of life. Dual-diagnosis OCD and ADHD can create a cyclical pattern where the symptoms of one condition exacerbate the symptoms of the other, creating a feedback loop of increasing distress. Understanding the nuanced relationship between these conditions is pivotal in crafting a holistic treatment approach.
OCD treatment
The journey to recovery from OCD is highly individualised, involving a blend of therapeutic interventions and, sometimes, medication. Early intervention often leads to better outcomes, with professional OCD treatment crucial for effectively managing the condition.
Cognitive Behavioural Therapy (CBT)
CBT is the gold standard in OCD treatment and a major aspect of UKAT London Clinic’s OCD programmes. It helps individuals face their fears head-on, better understand how thoughts influence behaviours and encourage them not to perform their compulsive rituals.
Family therapy
Involving family members in the therapeutic process can be very beneficial, helping them understand the condition better and learn how to support the individual effectively.
Mindfulness and meditation
Mindfulness, characterised by focused and non-judgemental attention to the present moment, offers a powerful tool for managing OCD symptoms. It fosters a grounded awareness of experiences and thoughts. Regular meditation practices can further reduce anxiety and stress levels, often heightened in individuals with OCD, resulting in a calming effect and decreased severity of symptoms.
Psychoeducation
This involves educating the affected individual on OCD intricacies and assisting them in understanding and managing their symptoms more proficiently.
Medication for OCD
Certain medications can also provide notable benefits for the symptoms of OCD, including selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants.
Lifestyle adjustments
Stress management techniques can be crucial in reducing the frequency and intensity of OCD symptoms. Similarly, regular physical activity has been shown to affect mental health, including in individuals with OCD positively.
Without treatment, OCD can become chronic, severely affecting the individual’s quality of life, impeding their ability to work, maintain relationships and perform daily tasks. Over time, controlling symptoms may become increasingly difficult as obsessions and compulsions become more entrenched.
UKAT London Clinic provides a haven for individuals suffering from OCD grounded in compassionate understanding, expertise and evidence-based treatment strategies. Our seasoned mental health professionals devise personalised OCD treatment plans that factor in the uniqueness of each individual’s experience and leverage a blend of psychotherapy, medication and holistic approaches. Contact us today to discover how we can help you effectively manage your OCD.

