Depression
Depression can be likened to a persistent shadow in your mind. It dims the colours of life, making everything seem dull. It feels as if a heavy weight is constantly pressing down on you, both mentally and physically, making even the simple tasks feel like an uphill battle. Depression steals your enthusiasm for life, leaving you feeling empty. But even in the darkest moments, there’s that glimmer of hope, that someday, that heaviness will lift, and you’ll find the strength to appreciate the simple joys life throws at you.
What is depression?
Depression, often referred to as a major depressive disorder (MDD), is a complex and debilitating mental health condition characterised by persistent feelings of sadness, hopelessness, and lack of interest or pleasure in previously enjoyed activities. It is more than a passing bout of sadness; depression is a pervasive and enduring condition that can significantly impact an individual’s thoughts, emotions and behaviour, often affecting quality of life.
What causes depression?
Depression is a complex mental health condition with multiple contributing factors. It often arises from a blend of biological elements, including neurotransmitter imbalances, genetic predisposition, and brain structure and function alterations. Environmental factors, such as trauma and chronic stress, can trigger or intensify depression, while certain psychological traits, medical conditions, substance misuse, hormonal shifts, and social isolation may also play a role. It’s essential to recognise that depression is highly individualised, meaning not everyone with risk factors will develop it, and those with depression may have distinct causes and triggers.
Diagnosing depression
The diagnosis of depression requires a comprehensive evaluation by a qualified mental health professional. While multiple criteria exist for diagnosis, primarily outlined in the Diagnostic and Statistical Manual of Mental Disorders, three major criteria are typically considered essential:
- Depressed mood: The primary criterion involves a consistently low or depressed mood for most of the day, nearly every day, lasting at least two weeks. This mood change must be noticeably different from the individual’s usual emotional state, characterised by feelings of sadness, emptiness, or hopelessness.
- Anhedonia: Anhedonia refers to a marked decrease or loss of interest or pleasure in almost all activities that previously brought joy or satisfaction. This includes hobbies, social interactions, and other activities that typically provide pleasure. Similar to the depressed mood criterion, anhedonia must persist for at least two weeks.
- Other symptomatic criteria: In addition to the core criteria of depressed mood and anhedonia, a diagnosis of major depressive disorder also requires the presence of at least four (or more) of the following symptoms during the same two-week period, representing a significant change from the person’s baseline functioning:
- Significant weight loss or gain (without dieting) or changes in appetite.
- Insomnia (lack of sleep) or hypersomnia (excessive sleeping).
- Psychomotor agitation (observable restlessness or slowed movements).
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive guilt.
- Diminished ability to concentrate or make decisions.
- Recurrent thoughts of death, suicidal ideation, or a suicide attempt.
Exploring the symptoms of depression
Depression is not just a transient emotional state but a mental health condition that can have profound and far-reaching effects on an individual’s well-being, relationships, and daily functioning. Here, we will delve into the various symptoms of depression to provide a comprehensive understanding of this condition.
Physical symptoms of depression:
- Fatigue
- Aches and pains
- Low libido
- Digestive issues
- Physical restlessness
- Slowed movements and speech
- Fluctuation in weight and appetite
- Cognitive difficulties
Behavioural symptoms of depression:
- Social withdrawal
- Reduced interest/pleasure
- Irritability and mood swings
- Substance abuse or addiction
- Indecisiveness
Understanding that depression is a condition with effective treatments is essential. Seeking help from a mental health professional, such as UKAT, is a crucial step in managing and recovering from the impact depression can have.
If you or someone you know is dealing with depression and also having thoughts of self-harm or suicide, it’s crucial to take immediate action.
What is a depressive episode?
A depressive episode, within the realm of mental health, denotes a distinct period when an individual undergoes a sustained and profound state of low mood or depression. It is a central feature in several mood disorders, including major depressive disorder (MDD), bipolar disorder, and persistent depressive disorder (formerly dysthymia).
Key characteristics of a depressive episode may include:
- Persistent Sadness: A pervasive feeling of sadness, emptiness, or hopelessness that lasts for most of the day, nearly every day.
- Loss of Interest or Pleasure: A significant decrease in interest or pleasure in activities that were once enjoyable, including hobbies, social interactions, and daily responsibilities.
- Changes in Sleep Patterns: Insomnia (difficulty falling or staying asleep) or hypersomnia (excessive sleep) can occur during a depressive episode.
- Fatigue: A notable decrease in energy levels and an overall feeling of exhaustion, even after adequate rest.
- Changes in Appetite or Weight: Significant changes in appetite may result in weight gain or loss.
- Difficulty Concentrating: Trouble focusing, making decisions, or maintaining attention on tasks.
- Feelings of Worthlessness or Guilt: Persistent feelings of self-doubt, guilt, or worthlessness, often without an apparent reason.
- Psychomotor Agitation or Retardation: Either feeling physically agitated and restless or experiencing slowed movements and speech.
- Suicidal Thoughts: In severe cases, individuals may have recurrent thoughts of death or suicide.
- Physical Symptoms: Some people may experience physical symptoms like aches, pains, headaches, or digestive problems in conjunction with their depressive episode.
The specific criteria for diagnosing a depressive episode can vary depending on the mental health classification system (e.g., DSM-5 or ICD-10) used by mental health professionals. To be diagnosed with a depressive episode, these symptoms must be present for a certain duration (usually at least two weeks) and significantly interfere with an individual’s daily functioning and well-being.
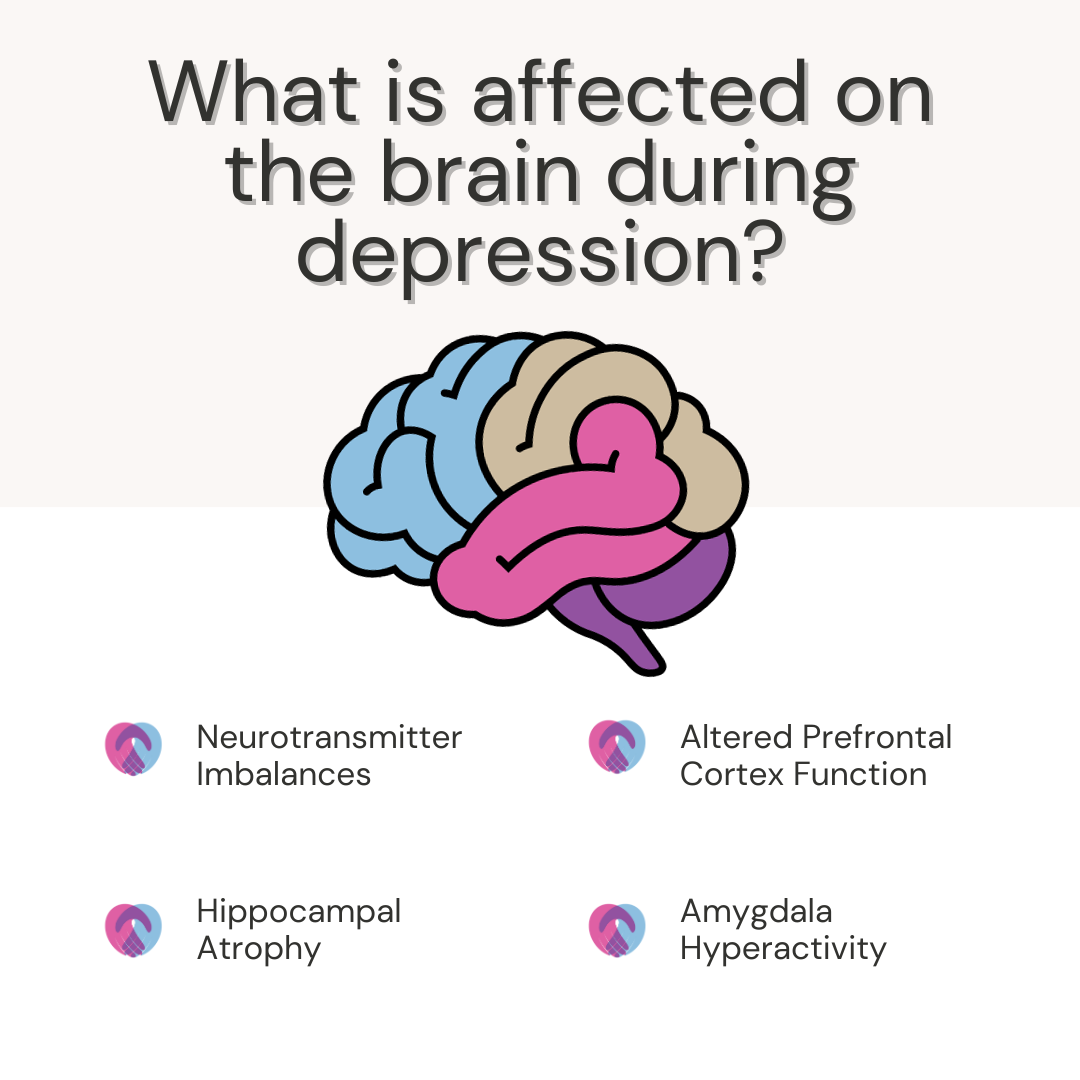
What happens to the brain during depression?
Depression can lead to various changes in the brain, although the exact mechanisms and patterns can vary.
Some of the key brain-related changes associated with depression include:
- Neurotransmitter Imbalances: One of the most widely recognised aspects of depression is alterations in neurotransmitters, which are chemical messengers that facilitate communication between nerve cells (neurons) in the brain. In depression, there often appears to be a deficiency in the availability of certain neurotransmitters, particularly serotonin, norepinephrine, and dopamine. These imbalances can affect mood regulation, contributing to sadness and hopelessness.
- Hippocampal Atrophy: The hippocampus, a brain region involved in memory and emotion regulation, may undergo structural changes during depression. Chronic stress, a common precursor to depression, can lead to atrophy or shrinkage of the hippocampus. This may impair memory and contribute to the emotional symptoms of depression.
- Altered Prefrontal Cortex Function: The prefrontal cortex, which plays a role in decision-making, concentration, and emotional regulation, may function differently in individuals with depression. There can be decreased activity in this region, leading to difficulties in cognitive functions and emotional control.
- Amygdala Hyperactivity: The amygdala is associated with emotional processing, including the response to stress and threats. In depression, the amygdala may become hyperactive, leading to heightened emotional responses, especially negative stimuli.
- Changes in Brain Connectivity: Studies using neuroimaging techniques like functional magnetic resonance imaging (fMRI) have shown altered patterns of brain connectivity in individuals with depression. These changes can affect how different brain regions communicate and may contribute to the emotional and cognitive symptoms of depression.
It’s important to note that these changes in the brain are not uniform across all individuals with depression, and the precise mechanisms underlying depression are still a subject of ongoing research. Additionally, while these changes are associated with depression, they are not the sole cause of the condition, which is influenced by a complex interplay of genetic, environmental, and psychological factors. Effective treatment approaches for depression often aim to restore neurotransmitter balance, reduce inflammation, and address the emotional and cognitive symptoms associated with these brain changes.
- Inflammation: There is increasing evidence linking inflammation to depression. Chronic inflammation in the body can affect the brain and may contribute to depressive symptoms. Elevated levels of inflammatory markers have been observed in some individuals with depression.
- Neurogenesis: In the past, the adult brain was believed not to produce new neurons (neurogenesis). However, recent research suggests that neurogenesis, particularly in the hippocampus, may still occur in adulthood and be impacted by depression. Reduced neurogenesis could affect mood regulation.
How do people overcome depression?
Treating depression is crucial to managing its symptoms and improving life quality. Effective treatments, such as therapy and medication, can alleviate the intense sadness, hopelessness, and despair accompanying depression. With the right treatment plan and support, many individuals experience significant relief from their symptoms, allowing them to regain their emotional well-being and functionality.
At UKAT London Clinic, we offer a diverse range of therapeutic solutions designed to support individuals in effectively managing depression. Some of the personalised therapeutic options you can explore with us include:
- Cognitive Behavioural Therapy (CBT): CBT is a highly effective psychotherapy approach for individuals dealing with depression. It focuses on identifying and challenging negative thought patterns, aiding in developing healthier thinking and behaviour patterns to manage and alleviate depressive symptoms.
- Family Therapy: Depression can affect the individual and their family dynamics. Family therapy can be pivotal in improving communication, fostering understanding, and enhancing support within the family unit. This, in turn, contributes to better outcomes for individuals grappling with depression.
- Mindful Healing: Holistic approaches like mindfulness meditation and art therapy are integral to our treatment offerings. These techniques provide individuals with valuable tools to manage stress, promote self-awareness, and enhance overall well-being in overcoming depression.
- Educational Support: Psychoeducation about depression, including its symptoms and effective management strategies, is pivotal for individuals and their support systems. Educational programmes can empower individuals to better understand and adhere to their personalised treatment plans, ultimately aiding their recovery.
- Immersive Experiences: At UKAT London Clinic, we also provide immersive therapeutic experiences, such as engaging with animals or nature in a controlled and supportive environment. These experiences, akin to equine therapy, facilitate self-awareness, improve interpersonal skills, and foster emotional regulation, complementing traditional therapeutic methods and offering a holistic approach to depression management.
It’s important to understand that while treatment can lead to substantial improvement and even remission of depression, it may not guarantee that depression will never return. Depression can be episodic, and some individuals may experience recurrent episodes. However, individuals can increase their resilience and manage future episodes by learning coping strategies, maintaining a healthy lifestyle, and staying connected with mental health professionals and support networks. In some cases, depression can indeed go into long-term remission, offering hope for a brighter and more stable future.
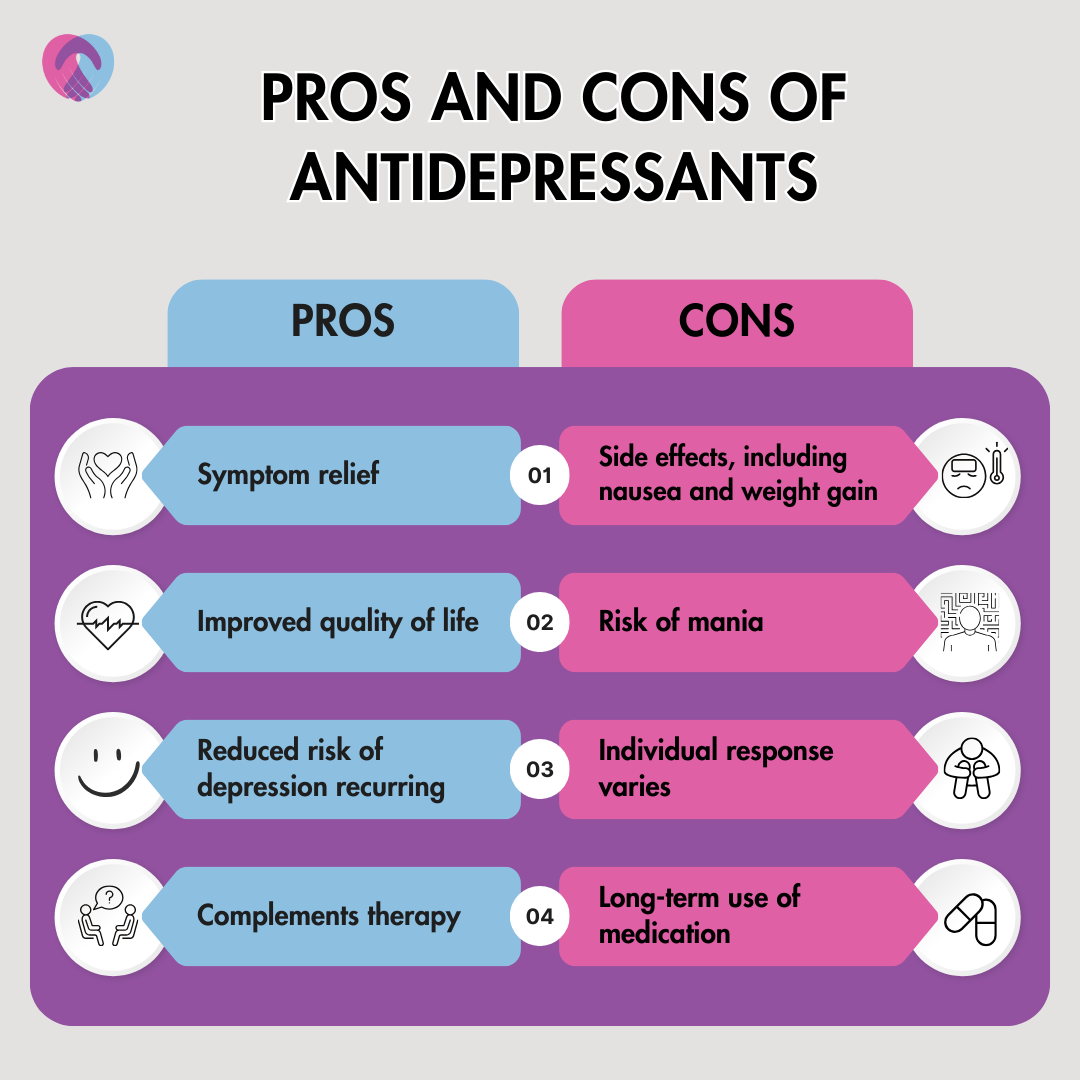
The affect antidepressants can have
Antidepressants vary in their effects and impact, with considerations including mood improvement for depression symptoms and reduced anxiety, especially with SSRIs. It’s important to note that they may take time to show full effects, and side effects like nausea and dizziness can occur. Responses differ among individuals, requiring trial and error under medical guidance.
Maintenance is often long-term, abrupt discontinuation can cause issues, and monitoring is crucial for bipolar individuals due to the risk of mania. In some cases, starting antidepressants may slightly raise the risk of suicidal thoughts, emphasising close monitoring. Tapering off gradually is recommended; therapy like CBT often complements medication for comprehensive depression treatment. Decisions should be made in consultation with healthcare providers, considering individual symptoms and medical history, with ongoing communication to ensure the best outcome.
Find out more today
UKAT London Clinic is here to provide comprehensive support for individuals grappling with depression. Our dedicated team of mental health professionals offers a range of evidence-based treatments, including psychotherapy and medication management, tailored to the unique needs of each individual. With a focus on holistic well-being, we aim to empower our patients with the tools they need to manage their symptoms and regain a sense of balance and hope.
Don’t hesitate to reach out to us to discover how UKAT London Clinic can be your partner in the journey towards recovery from depression.





