Bulimia
Bulimia nervosa is a serious yet sadly common eating disorder that profoundly impacts a person’s well-being and quality of life. Often misunderstood and mischaracterised, bulimia is more than just a problematic relationship with food; it intertwines deep-seated psychological distress with severe physical health risks. To grasp bulimia, we must consider the intricate interplay of emotions, behaviours, and societal pressures contributing to its development. By understanding its causes, symptoms, and effective treatments, we can provide vital support to those affected by this condition.
What is bulimia nervosa?
Bulimia nervosa is a potentially life-threatening eating disorder. The condition is characterised by a cycle of binge eating followed by compensatory behaviours, such as vomiting, excessive exercise or misuse of laxatives, to negate the calories consumed during the binge. This cycle often occurs in secret and is fuelled by an overpowering sense of guilt, shame and a fear of weight gain. The disorder often begins in adolescence or early adulthood and can affect individuals of any gender, race or background.
Bulimia symptoms and behaviours
The condition manifests through a range of bulimia symptoms and behaviours. Recognising the signs of bulimia as early as possible can make a huge difference in the success of bulimia recovery and treatment. Bulimia symptoms include:
Psychological bulimia symptoms
- Preoccupation with body size and shape: Individuals may constantly evaluate their bodies and experience dissatisfaction irrespective of their physical condition.
- Extreme fear of weight gain: Despite being in a healthy weight range, individuals may live in perpetual fear of gaining weight.
- Mood swings: Fluctuations in mood are common, and individuals might experience extreme irritability, depression or anxiety.
Behaviours
- Secrecy around eating: Individuals often prefer to eat alone and maintain secrecy around their eating habits to hide their condition.
- Binge eating: Engaging in episodes of eating a large amount of food quickly, often accompanied by a feeling of loss of control.
- Purge behaviours: Following a binge, individuals engage in behaviours such as forced vomiting, excessive exercise or misuse of laxatives to ‘undo’ the binge.
- Signs of self-induced vomiting: Frequent visits to the bathroom after meals, discarded packaging for laxatives or diuretics, and a smell of vomit are all potential signs of bulimia.
It is essential to note that these bulimia symptoms and behaviours can vary considerably between individuals, and not everyone with bulimia will experience all of them.
Bulimia health risks
Bulimia can pose a variety of significant health risks in the short and long term and can even lead to fatal consequences if untreated. The condition causes physical and mental health issues and can significantly impact relationships and socioeconomic well-being.
Physical bulimia health risks
- Gastrointestinal issues: The constant cycle of bingeing and purging can severely damage the digestive system, leading to acid reflux, stomach ulcers and irritable bowel syndrome.
- Electrolyte imbalance: Frequent vomiting can lead to a serious imbalance of vital electrolytes in the body, predisposing individuals to cardiac arrhythmias and muscle spasms.
- Dental problems: Exposure to stomach acid can cause dental erosion, gum disease and cavities.
- Hormonal imbalance: Bulimia can disturb hormonal balance, affecting menstrual cycles in females and lowering testosterone levels in males.
- Skin issues: Individuals might experience dry skin, brittle nails and hair loss due to poor nutrition.
- Bulimia face: This term refers to puffiness and swelling of the face, particularly in the jaw and cheek areas, due to repeated vomiting.
Mental health risks
- Depression: Many individuals with bulimia experience depressive symptoms, including persistent sadness and loss of interest in previously enjoyed activities.
- Anxiety: Bulimia can exacerbate anxiety, leading to a vicious cycle where anxiety triggers binge-purge behaviours, heightening anxiety levels.
- Low self-esteem: Constant preoccupation with body image and weight can foster low self-esteem and feelings of worthlessness.
- Suicidal thoughts: The distress and shame associated with bulimia can sometimes foster suicidal thoughts and behaviours.
Socioeconomic risks
Social isolation: Individuals with bulimia may isolate themselves from friends and family to conceal their eating habits.
Financial strain: The binge-purge cycle can often be financially draining, as individuals buy large amounts of food for binge episodes or miss work due to the strain of bulimia.
Recognising these health risks is a crucial step in understanding the grave implications of bulimia nervosa and underlines the importance of seeking timely intervention to prevent these complications and foster recovery.
Causes of bulimia nervosa
Bulimia nervosa has its roots in various factors, encompassing genetic and biological aspects, psychological predisposition and environmental and sociocultural influences. Understanding these underlying causes of bulimia nervosa can help craft a comprehensive treatment approach.
Genetic factors
Research shows a significant genetic predisposition towards developing bulimia nervosa, and having a close relative with the condition increases the risk substantially. Identifying specific genes is still under investigation, but twin studies have hinted at a substantial genetic component.
Biological factors
Biological factors include biochemical imbalances in the brain, particularly changes in the brain’s serotonin levels. These imbalances can influence a person’s mood, impulse control and eating habits.
Psychological factors
Psychological factors such as a perfectionist personality, low self-esteem and impulsive behaviour can all be precursors to developing bulimia. Individuals who have experienced trauma or abuse or have a history of substance abuse are also at a higher risk of developing eating disorders, including bulimia.
Sociocultural factors
Peer pressure, the societal pressure to maintain a certain body image and exposure to media that often propagates thin ideals can all contribute to the development of bulimia nervosa. Professions and activities that emphasise thinness, such as ballet and modelling, can also pose a higher risk.
Environmental factors
Growing up in a family with an excessive focus on weight, body shape and appearance can be a triggering factor, while personal experiences of bullying or criticism regarding your body can also foster the onset of bulimia. Individuals who have experienced stressful life events such as a loss or a major change may also find themselves more susceptible.
It is important to note that these causes can interact in complex ways, making each person’s experience with bulimia unique. Consequently, a holistic approach considering all these dimensions is pivotal in bulimia treatment and recovery.
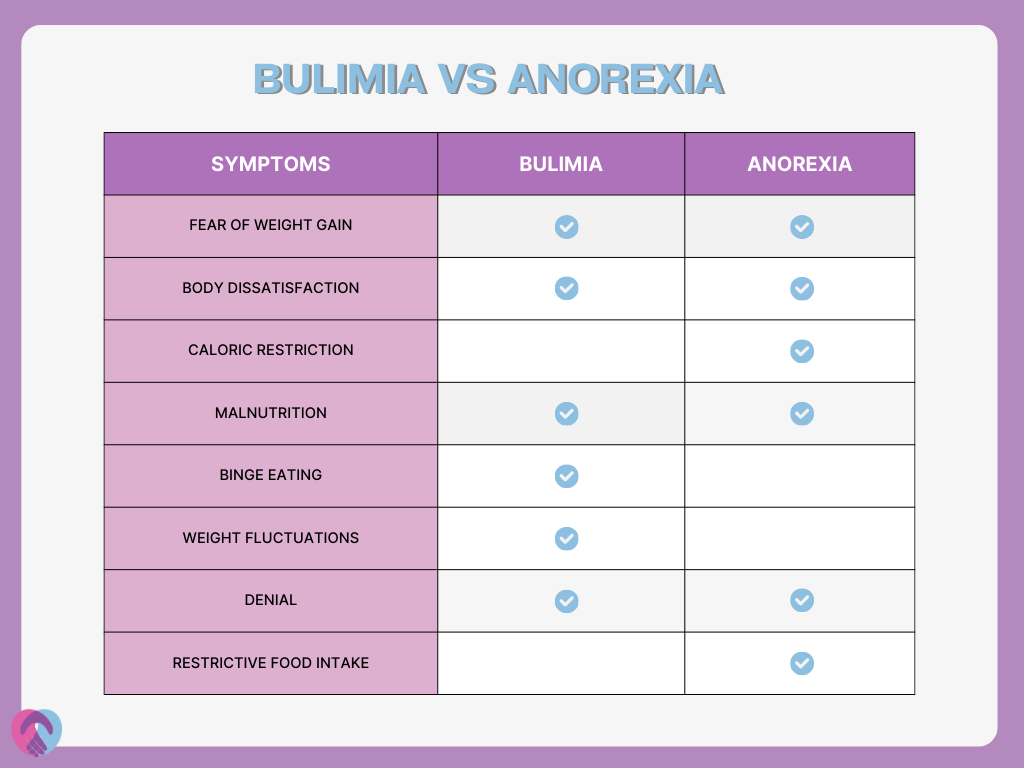
The difference between bulimia nervosa and anorexia
Bulimia nervosa and anorexia nervosa are both eating disorders with overlapping characteristics but also distinct differences that mark them as separate conditions. They share commonalities such as an intense fear of gaining weight, preoccupation with body size and shape, and often have a distorted body image. However, they primarily differ in how individuals approach eating and their subsequent behaviours.
While individuals with anorexia nervosa severely restrict their food intake, leading to significantly low body weight, those with bulimia nervosa engage in a cycle of binge eating followed by compensatory behaviours. People with bulimia nervosa are often at a normal weight with slight fluctuations, whereas anorexia nervosa causes dramatically low weight.
Bulimia can also have more noticeable physical symptoms such as swollen cheeks or jawline (bulimia face) and damaged teeth.
It is vital to note that despite these differences, both disorders share a central focus on body image and can often overlap, with individuals experiencing symptoms of both disorders.
The fundamentals of bulimia treatment
Effective bulimia treatment is a nuanced process involving a multidisciplinary approach to address the disorder’s psychological and physiological aspects. Therapy, nutritional guidance, lifestyle changes, and medication, when necessary, can all play their part in bulimia recovery and management.
Cognitive Behavioural Therapy (CBT)
CBT is a key aspect of UKAT London Clinic’s bulimia treatment programmes. CBT assists individuals in identifying and rectifying negative thought patterns and behaviours associated with bulimia. It helps recognise triggers for bingeing and purging and facilitates the development of healthier coping strategies.
Dialectical Behavioural Therapy (DBT)
DBT combines mindfulness and CBT techniques to help manage the emotional dysregulation often seen in bulimia nervosa. It teaches skills like mindfulness and distress tolerance, aiding in reducing the frequency of binge-purge cycles.
Family therapy
Family therapy works in tandem with individual therapy, offering education to family members on how to best support their loved ones during recovery. This can help repair relationships strained by bulimia and foster better understanding and a supportive home environment.
Holistic therapies
Bulimia is an all-encompassing condition, so holistic therapies can be crucial for healing on every level: physical, mental and emotional:
Mindfulness and meditation
These approaches foster self-awareness and self-acceptance, helping individuals to stay grounded and manage triggers more effectively.
Yoga
Incorporating yoga can aid in reconnecting the mind and body, promoting relaxation and reducing the anxiety often associated with bulimia nervosa.
Art and music therapy
Engaging in art and music therapy can offer a creative outlet for expression and has been found to have therapeutic effects in the treatment of various mental health conditions, including bulimia.
Nutritional counselling
Nutritional counselling involves working with a dietitian to foster healthy eating habits and develop a realistic and balanced meal plan. It is a vital pillar in recovery, nurturing a healthier relationship with food and body.
Support groups
Support groups and group therapy can provide peer support and a platform to share experiences, fostering a community that understands and aids in the healing bulimia recovery journey.
Bulimia medications
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs, like fluoxetine, have been found to be beneficial in reducing the symptoms of bulimia, especially when combined with psychotherapy.
Antipsychotics
In certain cases, antipsychotic medications may be prescribed as adjunct therapy to help manage severe symptoms or co-occurring mental health issues.
When to seek help?
Recognising the right time to seek help can be vital to recovery from bulimia nervosa. Many individuals grappling with bulimia find it challenging to come forward for various reasons, including shame, denial or fear of judgement. However, early intervention can significantly enhance the chances of bulimia recovery. Here are some indicators that it might be time to seek help:
- Increasing preoccupation with body image: If you find yourself or a loved one increasingly preoccupied with body weight, shape or appearance, it may be a sign to seek professional guidance.
- Physical symptoms: The onset of physical symptoms such as dental problems, chronic sore throat and gastrointestinal issues signal that the body is in distress and needs medical attention.
- Emotional distress: This includes depression, anxiety and irritability.
- Isolation: Individuals with bulimia often isolate themselves to conceal their eating habits.
- Impact on daily life: When bulimia affects daily life significantly and interferes with work, school or relationships, it is time to seek help.
- Recognition of unhealthy patterns: Primarily, binge eating followed by compensatory behaviours, like forced vomiting or excessive exercise.
Recovery from bulimia nervosa is a gradual, step-by-step process requiring patience, perseverance and commitment. Every individual has a unique path to recovery and requires a tailored treatment plan that adapts to their changing needs and progresses.
By adopting a multipronged approach to treatment, encompassing psychotherapy, medication management and holistic therapies, UKAT London Clinic guides individuals on the path to bulimia recovery. It is a journey of rediscovery and rebuilding, with the end goal being a healthy, fulfilling life post-recovery. Call us today to find out more.

