Bipolar Disorder
Bipolar disorder, characterised by severe mood swings, profoundly impacts all aspects of an individual’s life, including daily functioning, relationships, job performance, and prospects. These unpredictable shifts often lead to misconceptions, emphasising the importance of understanding the breadth of bipolar disorder symptoms for diagnosis and effective management. While navigating life with bipolar disorder may pose a daily struggle, providing suitable treatment and steadfast support can empower individuals to seize control and embark on a path towards enduring stability and fulfilment.
What is bipolar disorder?
Bipolar disorder, formerly referred to as manic depression, is a mental health condition characterised by extreme fluctuations in mood, energy, and activity levels. These fluctuations oscillate between periods of heightened energy and activity (manic episodes) and periods of low energy and deep sadness (depressive episodes), often punctuated with periods of normal mood.
What are the symptoms of bipolar disorder?
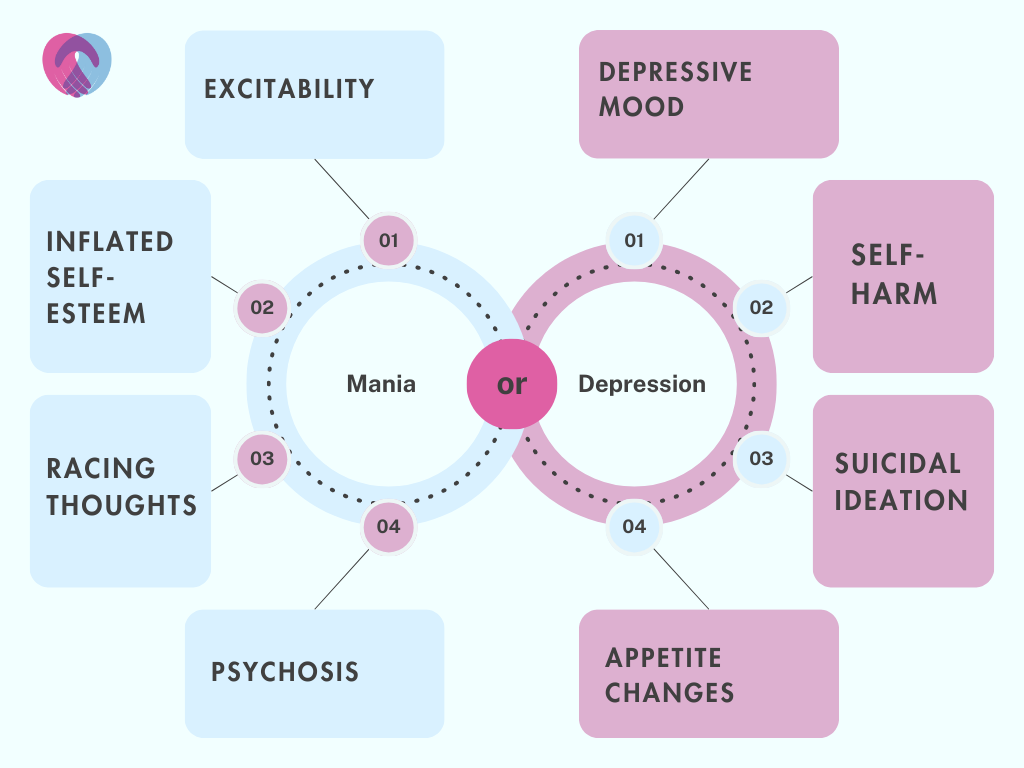
Distinct episodes of mania and depression characterise bipolar disorder, each with its unique set of symptoms.
Manic episodes
Manic episodes involve a period where individuals experience an excessively elevated, expansive or irritable mood. Being able to identify manic bipolar disorder symptoms can be a crucial step in getting timely help for individuals experiencing a dangerous episode and preventing any severe consequences:
- Over-enthusiasm and excitability: Individuals may exhibit an unusual level of enthusiasm and excitability, getting highly animated and passionate about ideas or projects which are unrealistic or overambitious.
- Inflated self-esteem: Individuals may perceive themselves as superior to others, sometimes bordering on delusional levels of self-importance. In extreme cases, they may develop grandiose plans, believing they have special connections with prominent figures or divine entities.
- Racing thoughts: Individuals frequently experience racing thoughts that rapidly leap from one topic to another. This mental state can make concentrating on a single task difficult, leading to fragmented and unproductive work output.
- Increased engagement in pleasurable activities: There is often a notable increase in potentially risky activities that bring pleasure, including heightened sexual drive, reckless spending or engaging in daring endeavours. However, these impulsive behaviours tend to have a high potential for harmful consequences.
- Agitation and irritability: Apart from an elevated mood, individuals may experience periods of turmoil and irritability, finding themselves easily angered or frustrated, resulting in conflicts and strained relationships with people around them.
- Physical symptoms: Manic episodes may also bring about physical symptoms such as increased energy and decreased need for sleep. However, this can lead to poor decision-making due to mental and physical exhaustion.
- Psychosis: In severe manic episodes, individuals can lose touch with reality, experiencing hallucinations (seeing or hearing things that others do not) or delusions (holding beliefs that are not based on reality). This state requires immediate medical attention as it can be highly distressing and potentially dangerous for individuals and others around them.
Depressive episodes
Depressive episodes represent the polar opposite of manic episodes in the bipolar disorder spectrum. These periods are marked by a profound sadness or a loss of interest or pleasure in most activities. Again, being able to recognise these severe symptoms is crucial for both individuals with bipolar disorder and their support networks to prevent the most dire outcomes:
- Depressed mood and loss of interest: During a depressive episode, individuals undergo a sustained period of sadness or hopelessness, finding it hard to derive joy from things they once enjoyed. This pervasive downcast mood permeates all aspects of life, affecting relationships, social lives and work performance.
- Changes in appetite: Depressive episodes often alter eating habits significantly, leading to weight gain due to excessive eating or weight loss stemming from a lack of interest in food. These changes in appetite are not linked to dieting or physical health efforts but are instead a symptom of the depressive state.
- Self-harm: This can be in the form of physical harm such as cutting, burning, or hitting oneself or engaging in risky behaviours that indirectly cause harm. It is a critical symptom, representing a severe manifestation of the disorder, necessitating immediate intervention and ongoing support to ensure the individual’s safety.
- Suicidal ideation: Unfortunately, individuals in a depressive state might have recurrent thoughts of death, self-harm or suicide. These thoughts can range from passive ideas about death to forming concrete plans for suicide. This symptom represents a severe risk, and it is crucial to take any sign of suicidal ideation seriously, with immediate intervention being paramount.
Types of bipolar disorder
Understanding the complexity of bipolar disorder requires a deep exploration of its various subtypes, each distinguished by specific patterns of mood fluctuations and severity of bipolar disorder symptoms. These distinctions are not merely academic; they allow clinicians to craft treatment plans tailored to the individual’s experiences, paving the path for more successful management of the condition.
Bipolar I disorder
Bipolar I disorder is characterised by at least one manic episode, which may or may not be followed by a depressive episode.
Bipolar II disorder
Bipolar II disorder, on the other hand, involves a history of one or more major depressive episodes accompanied by at least one hypomanic episode. A hypomanic episode shares many characteristics of a manic episode but is less severe and does not impede daily functioning to the same extent.
Cyclothymic disorder
People with this disorder experience chronic fluctuations in mood that alternate between hypomanic and depressive symptoms but do not meet the full criteria required to diagnose manic or depressive episodes. The diagnosis requires these symptoms to persist for at least two years in adults or one year in children and adolescents. While the symptoms may appear milder than those seen in bipolar I and II disorders, cyclothymic disorder can still significantly affect an individual’s quality of life.
Rapid-cycling bipolar disorder
This is not a standalone subtype but is used to describe a situation where an individual experiences four or more episodes of mania, hypomania or depression within twelve months. Rapid cycling introduces an added layer of complexity to treatment and management, as the frequent shifts in mood can be particularly distressing and disruptive to individuals’ lives.
Other specified and unspecified bipolar and related disorders
In addition to the above classifications, there are cases where an individual exhibits some symptoms of bipolar disorder but does not fully meet the criteria for any of the above subtypes
Stages of bipolar disorder
There are different representations of bipolar disorders, but three main stages represent the cycle most people experience: the prodrome stage, the acute stage and the maintenance stage. These stages delineate the phases that individuals living with bipolar disorder typically navigate through, each exhibiting distinct characteristics and requiring specific approaches for management.
Prodrome phase
In the prodrome phase, individuals experience subtle changes in their mood, energy levels and behaviour, signalling the onset of a manic or depressive episode. This stage may involve symptoms such as sleep disturbances, shifts in appetite and slight mood swings, which are not yet intense but indicate that a more severe episode is forthcoming. It is a crucial stage for initiating early interventions to prevent a full-blown episode possibly.
Acute phase
The acute phase marks the occurrence of the full-fledged manic or depressive episodes described above. Recognising and addressing the symptoms promptly during the acute phase is vital to safeguard the individual’s well-being and prevent further complications.
Maintenance phase
Following an acute episode, individuals enter the maintenance phase, where the primary goal is to prevent the recurrence of severe episodes. During this stage, individuals need to work closely with medical professionals, focusing on building resilience and fostering a supportive environment. This will help them lead a more balanced life, effectively managing the highs and lows.
What causes bipolar disorder?
The causes of bipolar disorder are multifaceted, encompassing a blend of genetic, environmental and physiological influences. Research into bipolar disorder has made significant strides in recent years, with the findings playing a crucial role in effectively managing and treating the condition.
Genetic factors
There is compelling evidence pointing to a genetic predisposition in the onset of bipolar disorder, with research involving identical twins documenting a notably higher rate for bipolar disorder than non-identical twins. This is a clear indicator of the genetic influences at play in the development of the condition.
Environmental factors
Environmental factors also contribute to the onset and exacerbation of bipolar disorder. Various external triggers can precipitate episodes of mania or depression, including trauma and grief. Substance abuse and addiction are also intrinsically linked to bipolar disorder, with individuals seeking relief from their symptoms in drugs or alcohol or engaging in risky substance use behaviours.
Physiological factors
Various physiological factors can influence the onset and progression of bipolar disorder. Disruptions in the balance of neurotransmitters, the brain’s chemical messengers, have been identified as one potential cause as neurotransmitter imbalance affects mood regulation, instigating manic or depressive episodes. Hormonal fluctuations, including thyroid dysfunction and other endocrine disorders, can also significantly affect an individual’s mood, presenting triggers for bipolar episodes.
Treatment for bipolar disorder
Effective treatment for bipolar disorder requires a multifaceted approach that often combines therapy, medication and lifestyle modifications.
Cognitive Behavioural Therapy (CBT)
CBT is crucial in treating bipolar disorder, leveraging the deep-seated connection between thoughts, feelings and behaviours to forge pathways towards stability. At its core, CBT encourages individuals to replace negative thought patterns with more balanced perspectives, encourages participation in enjoyable activities and provides individuals with the tools to anticipate and navigate potential triggers for manic or depressive episodes.
Dialectical Behaviour Therapy (DBT)
This offers a multifaceted approach to treating bipolar disorder. DBT facilitates emotional regulation, aiding individuals in understanding and managing their emotions more proficiently to foster stability and incorporates mindfulness strategies that can enhance interpersonal effectiveness and improve relationship distress tolerance.
Family therapy
Family therapy can also be pivotal, fostering a supportive environment through open communication and understanding. This approach endorses open dialogue and problem-solving techniques to reduce stress, educate loved ones about bipolar disorder and promote harmony through communication enhancement training.
Medication management
Medications are another cornerstone of treatment for bipolar disorder, helping to stabilise mood and manage symptoms. Mood stabilisers are often the first line of treatment, assisting in controlling manic or hypomanic episodes and preventing relapses. Atypical antipsychotics can be effective in managing both manic and depressive episodes, while antidepressants can help individuals to manage depressive symptoms.
Lifestyle modifications
Lifestyle modifications can also enhance the effectiveness of medical and psychotherapeutic treatments. Regular physical activity can aid in stabilising mood and reducing symptoms of depression, while a balanced diet can support overall well-being and potentially moderate the symptoms of bipolar disorder.
UKAT London Clinic provides bespoke, comprehensive treatment plans that help our clients effectively manage symptoms, prevent relapses and have more stable and fulfilling lives. Our therapists and mental health experts provide a full medical assessment and guide our clients in navigating the myriad complexities of bipolar disorder. Utilising a multi-disciplinary approach, our team offers an integrated regimen comprising therapy and lifestyle interventions grounded in the latest scientific research and evidence-based practices.


