Binge Eating Disorder
Binge Eating Disorder (BED) is the most common eating disorder, affecting 1 in 50 people, surpassing the combined prevalence of bulimia and anorexia nervosa. This complex disorder intersects mental and physical health, resulting in a debilitating cycle. Despite its prevalence, BED often receives less attention. However, a comprehensive understanding of its symptoms, triggers, and treatment options can pave the way to effective recovery.
What is binge eating disorder?
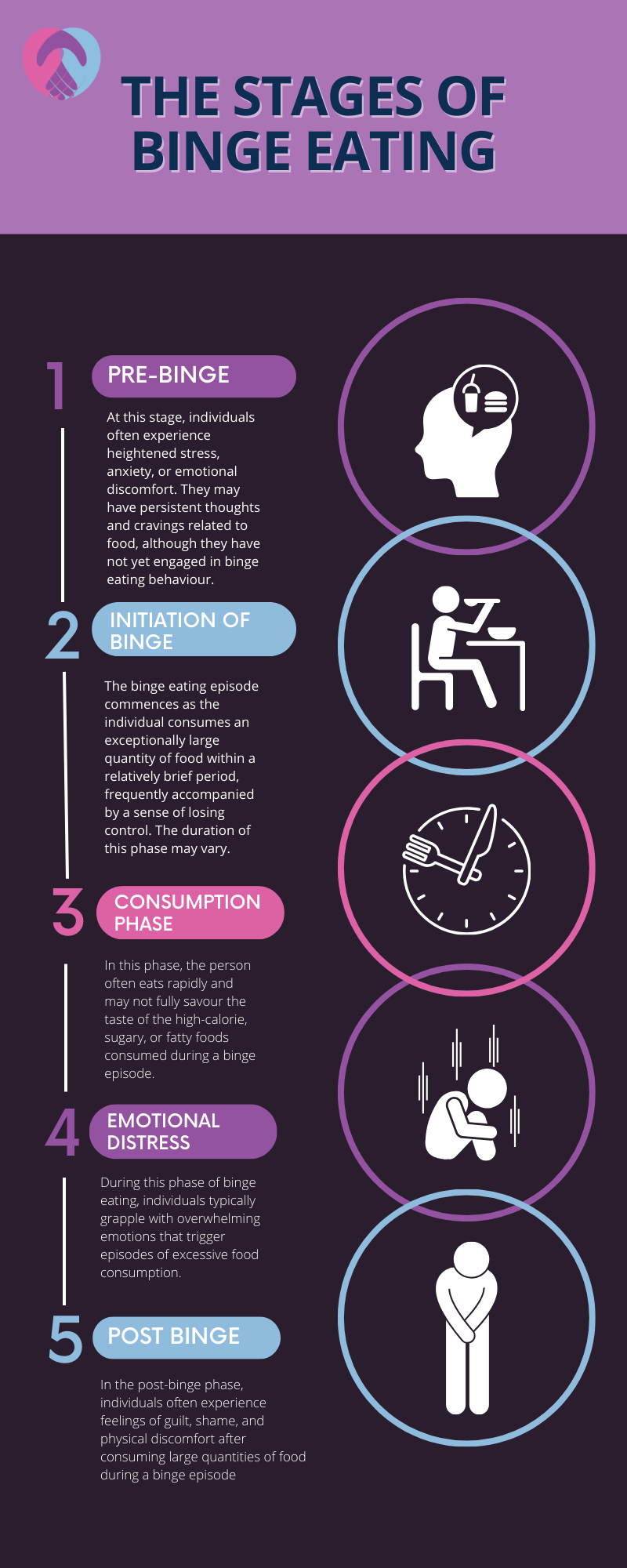
Binge eating disorder, also sometimes called food addiction or compulsive overeating, is characterised by recurrent episodes of eating large quantities of food, often very quickly and to the point of discomfort. Individuals with BED lose control during these episodes and are unable to stop eating even though they don’t need to. It is vital to differentiate BED from occasional overeating, as BED involves more frequent and intense experiences, often accompanied by distress, shame and a feeling of loss of control.
While Binge Eating Disorder (BED) can impact individuals from diverse backgrounds, it’s important to highlight that BED is more prevalent among men compared to anorexia and bulimia. Unfortunately, a considerable number of individuals with BED do not seek treatment, a rate significantly lower than that seen in other eating disorders.
This lack of seeking assistance can be attributed to various factors, including the stigmatisation associated with the disorder and a lack of understanding and awareness about its severe implications on health. It is a silent epidemic, largely because societal norms around food consumption can sometimes mask the severity of BED, and the emphasis on dieting in many cultures can further exacerbate the disorder.
Causes of binge eating disorders and food addiction
Understanding the causes of BED is complex as it involves a wide range of genetic, biological, psychological and environmental factors. However, all of these factors must be considered to create a compassionate, effective approach to treatment:
Genetic factors
Research suggests BED can run in families, highlighting a potential genetic predisposition. While no specific “BED gene” has been identified, individuals with a family history of eating disorders are at a higher risk of developing the disorder.
Biological factors
Biological aspects, such as irregularities in the brain or chemical imbalances, may foster BED development. One theory is that individuals with BED may have a differently functioning hypothalamus, which affects appetite regulation and leads to compulsive overeating.
Psychological factors
A substantial number of individuals with BED suffer from comorbid mental health issues such as depression, anxiety or bipolar disorder. Emotional trauma, stress and body dissatisfaction also often precede BED with psychological interventions forming a pivotal part of treatment.
Environmental and social factors
The environment an individual is exposed to, the societal norms regarding body image and their relationship with food can significantly influence the development of BED. Societies that vehemently promote thinness can indirectly foster BED by encouraging restrictive dieting, leading to binge episodes.
Binge eating symptoms and behaviours
Binge eating disorder causes unique symptoms and behaviours, distinct from other eating disorders. Recognising these can be a pivotal step towards seeking help and beginning the recovery journey.
- Rapid eating
- Eating even when not hungry
- Frequent episodes of uncontrolled eating
- Eating in secret
- Feeling distressed during and after binge eating
- Eating until uncomfortably full
- Frequently dieting
- Fluctuations in weight
- Preoccupation with body shape and weight
Common triggers for binge eating episodes
While BED triggers can vary significantly from individual to individual, some common factors tend to provoke binge eating episodes. Understanding these common triggers can be vital in formulating a strategy to prevent binge eating episodes and foster a path towards binge eating recovery.
Emotional triggers
- Stress: High-stress levels can often lead to binge eating, as people might use food as a coping mechanism.
- Depression: Feeling low and depressed can sometimes provoke a binge eating episode as an attempt to find comfort in food.
- Anxiety: Individuals experiencing anxiety might resort to binge eating to alleviate their symptoms momentarily.
Psychological triggers
- Low self-esteem: Individuals with low self-esteem might binge eat as a form of self-punishment or seek comfort.
- Boredom: A lack of engaging activity can sometimes lead individuals to binge to pass the time.
Social triggers
- Social isolation: Feeling isolated and lonely can sometimes drive individuals to seek comfort through binge eating.
- Peer pressure: Being pressured by peers to eat more or engage in unhealthy eating habits can sometimes trigger a binge eating episode.
Environmental triggers
- Availability of food: Having easy access to large quantities of food can sometimes facilitate binge eating episodes.
- Advertisements: Being constantly bombarded with food advertisements can sometimes ignite cravings, leading to binge eating.
Physical triggers
- Skipping meals: Skipping meals can lead to extreme hunger, triggering a binge eating episode.
- Hormonal fluctuations: Changes in hormone levels can sometimes affect appetite, potentially leading to binge eating.
Binge eating disorder health consequences
Binge eating can lead to a series of adverse health outcomes affecting both the physical and psychological aspects of a person’s well-being. Understanding these health complications illustrates the urgency to seek professional help for binge eating as soon as possible.
Physical health complications
- Obesity: While not everyone with BED is obese, many individuals with the disorder tend to be overweight due to the consistent overconsumption of calories. This situation raises the risk of obesity-related health complications.
- Digestive issues: Regular binge eating episodes can lead to digestive problems, including gastrointestinal distress, acid reflux and irritable bowel syndrome.
- Cardiovascular diseases: BED increases the risk of developing high blood pressure, high cholesterol levels and heart diseases stemming from the frequent intake of large quantities of fat and sugar.
- Type 2 diabetes: BED can elevate the risk of developing type 2 diabetes due to obesity and the irregular intake of high-sugar foods.
Mental health complications
- Depression and anxiety: Individuals with binge eating disorder often experience a cyclical pattern of compulsive eating and guilt, which can develop depression and anxiety disorders.
- Low self-esteem and body dissatisfaction: The disorder often leads to a negative body image and lowered self-esteem as individuals become increasingly dissatisfied with their appearance.
- Sleep disorders: BED can also influence sleep patterns adversely, leading to insomnia and sleep apnea.
Other health concerns
- Musculoskeletal problems: Over time, binge eating can lead to issues with the musculoskeletal system, including joint pains and mobility issues, due to increased weight and obesity.
Gallbladder disease: There is an increased risk of developing gallbladder diseases due to the frequent fluctuation in weight often associated with BED.
Diagnosing binge eating disorder
Diagnosing binge eating disorder is a comprehensive process that entails meticulous assessment of an individual’s medical history, physical health and psychiatric status. Diagnosis is laid out in the DSM-5 to help clinicians identify the condition and begin the BED recovery process.
DSM-5 diagnostic criteria
The DSM-5 recognises binge eating disorder as a distinct clinical condition, which is crucial in ensuring that individuals receive the appropriate treatment and support. The main criteria for diagnosing BED according to DSM-5 include:
- Recurrent episodes of binge eating: This is characterised by eating an unusually large amount of food quickly and lacking control during the binge episode.
- Distress regarding binge eating: Individuals must experience marked distress regarding their binge-eating episodes.
- Frequency of binge eating episodes: The binge-eating episodes occur, on average, at least once a week for three months.
- Absence of compensatory behaviours: Unlike other eating disorders, BED does not involve regular compensatory measures such as vomiting or excessive exercise to counter compulsive overeating.
Psychological and physical assessments
Beyond the criteria mentioned, healthcare professionals may carry out a series of assessments to establish a diagnosis, which might include:
- Physical examination: A detailed physical examination is carried out to identify any physical complications arising from BED.
- Psychiatric evaluation: To understand the depth of the disorder, a psychiatric evaluation involving detailed discussions about eating habits, mental health conditions and the emotional factors linked with eating can be performed.
- Nutritional assessment: A nutritional assessment to evaluate the individual’s dietary habits and nutritional intake is often part of the diagnostic process.
Collaborative efforts: Diagnosing BED involves a collaborative effort where a team of healthcare providers, including psychiatrists, psychologists and dietitians, work together to understand the multifaceted nature of the disorder.
Binge eating disorder treatment
For successful binge eating recovery, fostering a healing environment that encourages a healthy relationship with food while addressing underlying psychological issues is essential. The treatment process for binge eating may involve:
Therapeutic approaches
- Cognitive behavioural therapy (CBT): CBT remains the most evidence-based treatment for BED and is a key aspect of binge eating recovery at UKAT London Clinic. CBT aids individuals in understanding the link between their thoughts, feelings and behaviours and developing strategies to alter negative patterns.
- Dialectical behaviour therapy (DBT): DBT can help regulate emotions and reduce the frequency of binge eating episodes by teaching individuals skills like mindfulness and distress tolerance.
- Family therapy: This involves working with families to develop strategies to support the individual recovering from BED. Family therapy can help to foster understanding and create a supportive home environment that encourages binge eating recovery.
Holistic therapies
In addition to standard treatments, holistic therapies such as yoga, meditation, and acupuncture can benefit recovery. These therapies focus on healing the whole person – body, mind and spirit.
Nutritional counselling
At UKAT London Clinic, our expert nutritionists are a vital part of the recovery process. They help our clients craft a diet plan that encourages a healthy relationship with food and teaches them about nutritional needs and how to make healthier food choices.
Medication
Medication may sometimes be prescribed as part of the treatment plan. Common medications include:
- Antidepressants: They can help manage symptoms of depression and anxiety that often co-occur with BED.
- Antiepileptic drugs: Some medications initially developed to treat epilepsy have shown promise in reducing binge eating episodes.
At UKAT London Clinic, a successful recovery from BED involves not just the cessation of binge eating episodes but also fostering a healthy relationship with food and yourself. Our expert binge eating recovery team guides our clients in learning to eat mindfully, regaining control over eating behaviours and nurturing a positive self-image. Through continued therapy and support, individuals can learn to lead fulfilling lives free from the grips of binge eating disorder.

